▶ Watch Video: How public health works – and why it sometimes doesn’t
Monkeypox is now spreading around the world, and is putting the U.S. public health system once again on the front lines in a battle to keep the country safe.
When asked if monkeypox represents another pandemic like COVID-19, Dr. Rochelle Walensky, director of the Centers for Disease Control and Prevention, said the CDC has been responding aggressively, educating health professionals and patients alike. “We have been working extraordinarily hard, and we are still in a position where we can contain this,” she said.
CBS News chief medical correspondent Dr. Jonathan LaPook asked, “There’s no crystal ball, of course, but do you see monkeypox getting out more widely to the general population?”
“I think we are going to see more cases before we see less, and that is because we will have more testing,” she replied. “We have more education out there, people know what they’re looking for and how to test for it.”
The total of monkeypox cases in the U.S. has been growing steadily and is now more than 2,800. While anyone can get monkeypox, the virus is spreading predominately among gay, bisexual, and other men who have sex with men.
Walensky said, “To our knowledge right now, it does look like most of the transmission is happening with close, personal contact.”
With the U.S. public health system front-and-center, “Sunday Morning” thought this would be a good time to explore what the system actually does.
LaPook asked Michelle Williams, dean of faculty at the Harvard T.H. Chan School of Public Health, “Why is public health different than the practice of medicine?”
“In medicine, it’s the individual that’s the patient; in public health, you can think of the individual, the community, the planet as the patient,” she replied.
Williams said the estimated 270,000 public health workers in this country are unsung heroes, who aren’t valued enough because the public takes their contributions for granted. “When public health works, nothing bad happens. So, you don’t notice that that child that had a spill on the bicycle got up and is just fine because they’re wearing a helmet,” she said.
Public health workers have a lot on their plate, including eliminating disease; cutting down on workplace injuries; ensuring clean water and better sanitation; reducing injuries from fires and car crashes; and keeping our food safe to eat.
Tre Williams, a health inspector in Oklahoma City, showed LaPook how he goes about his job during a visit to a restaurant: “Here I’m checking to make sure he’s not stacking dishes. You know, if you stack wet dishes on top of each other, it builds up bacteria. We don’t want that.”
“This is the kind of stuff that the general public has no idea about, right? They’re not seeing this?” asked LaPook.
“Right, right. Absolutely.”
America’s public health system has a long history. In 1799, Boston set up one of the country’s first health departments, led by none other than Paul Revere.
Since 1900, advances in health and safety have increased U.S. life expectancy by an estimated 25 years.
Still, during the COVID pandemic, local health departments have had to scramble and improvise. In Oklahoma City, Patrick McGough, who heads the City/County Health Department, explained their program for vaccines, boosters and flu shots. “We’re providing this service free to the public. People just drive on through. They don’t have to have an appointment, nothing! It’s warmer, it’s friendly, you’re in your own car.”
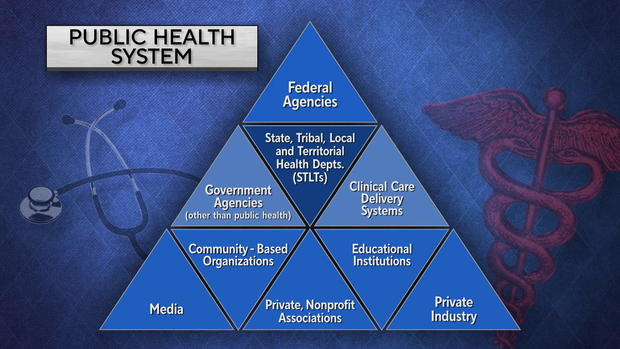
The structure of the public health system is extremely complex: local and state departments, educational institutions, private industry, and at the top government agencies like the Department of Health and Human Services, the National Institutes of Health, the CDC, and the FDA. No one person runs the whole system, and not every branch has the resources it needs.
For example, the technology to securely share health information electronically has existed for decades, yet at the height of the pandemic, doctors were faxing orders for COVID tests to the Oklahoma City/County Health Department.
LaPook asked, “Why in the world would anybody still need to use a fax?”
“Basically it’s about the doctors’ offices,” McGough replied. “They don’t all have secure forms of transferring information about you as a patient.
“We need a health care information exchange that is just at our fingertips, that the health departments and the hospitals and the primary care physicians can all share information so quickly and easily,” he said.
But that’s not what we have. Instead, there’s a patchwork of reporting systems across the country that don’t effectively talk with each other – critical during the early stages of outbreaks like COVID and monkeypox.
And, Dr. Walensky said, there are more challenges. When asked if the CDC has the authority to demand public health agencies around the country send information to it, she replied, “We do not.”
In fact, reporting cases from around the country is voluntary.
- Florida, other states, scale back virus reporting just as COVID cases surge
- Massachusetts will stop daily COVID case count report, switch to weekly
- CDC stops monitoring COVID-19 cases on cruise ships
- Latest Bay Area COVID-19 surge comes as fewer report test results
LaPook asked, “Do the data systems exist right now to adequately collect all the information needed?”
“They don’t,” Walensky said. “We’ve made a lot of progress during COVID, but we still have a lot of work to do. It would really be helpful if we had the capacity, the data systems, the workforce, the laboratory systems in place, the public health infrastructure truly in place, so that we could deliver health to all of America.”
“Why don’t we have those systems in place right now?”
“There has been a chronic, decades-long underfunding of a public health infrastructure in America,” she replied.
And Michelle Williams said the public health system faces a brain drain. “We know that burnout is real and pervasive,” she said.
When asked when was his last vacation, Patrick McGough responded: “Um, I haven’t had a vacation.”
It’s estimated that since 2008, at least 38,000 state and local public health jobs have disappeared.
The collision of public health and politics hasn’t helped. In Oklahoma City, McGough is feeling the heat. “Yes, lots of hate mail, lots of hate email, texts that were awful, all kinds of stuff,” he said.
- Public health workers report being threatened and harassed during the pandemic
- Health care workers say they’re facing verbal and physical abuse amid spread of COVID misinformation
- Hundreds of Missouri health care workers are getting personal panic buttons to combat increased workplace assaults
LaPook asked, “So, when people question your motives, what does that feel like?”
“I see that I have staff on the front lines giving everything they have: their family time, their own health, their own finances. And then to be attacked and called all kinds of things, it didn’t just happen because the pandemic arrived. Something else happened. Something caused people to lose faith. And it’s to the public’s demise. It may do away with public health.”
Despite these challenges, Michelle Williams is seeing at Harvard makes her optimistic: a year-over-year 50% increase in applications to their public health school.
How do you explain that? “They are running towards the opportunity to have an impact in this world,” she said. “And I am inspired by that. Because we are going to prevail. It will take more time, but we are going to prevail.”
For more info:
- Dr. Rochelle Walensky, director, Centers for Disease Control and Prevention
- Michelle Williams, dean of faculty, Harvard T.H. Chan School of Public Health
- Oklahoma City/County Health Department
Story produced by Jay Kernis and Julie Kracov. Editors: Joseph Frandino and George Pozderec.